Good documentation is the backbone of quality healthcare. It shapes communication and streamlines your billing process. If you are a clinic owner or team lead, you know that the correct note format makes everything run smoothly. So, should you choose SOAP or DAP?
The Importance of Clear Notes
Accurate records don’t just protect your practice; they improve care and simplify audits. Structured notes can cut medical errors by up to 30%. Your team works better with a note template that fits their routines and meets compliance needs.
What Are SOAP Notes?
SOAP stands for Subjective, Objective, Assessment, and Plan. This format has been a staple in clinical documentation for decades, especially in medical, nursing, and mental health settings.
- Subjective: What the patient reports about their symptoms or feelings.
- Objective: What the provider observes or measures; vital signs, lab tests, or physical findings.
- Assessment: The professional’s interpretation or diagnosis based on the information.
- Plan: The next steps for treatment, tests, follow-ups, or referrals.
The strength of SOAP notes is in their clear structure. They help healthcare providers keep the patient’s own words and medical facts separate. This makes SOAP notes very useful for tracking detailed medical cases or when it’s important to show how a diagnosis was made.
What Are DAP Notes?
DAP stands for Data, Assessment, and Plan. This format streamlines documentation by focusing on the essentials:
- Data: All relevant information from the session, including patient statements and observable details.
- Assessment: The provider’s clinical impressions and insights.
- Plan: The outlined next steps for care.
You can say DAP as a more compact version of SOAP. It avoids the strict separation of subjective and objective data, which saves time for providers who don’t need such a rigid distinction.
SOAP vs. DAP
|
Feature
|
SOAP Notes
|
DAP Notes
|
|
Structure
|
Four sections: Subjective, Objective, Assessment, Plan
|
Three sections: Data, Assessment, Plan
|
|
Detail Level
|
High, separates patient voice from clinical facts
|
Moderate, combines observations and patient input
|
|
Time to Complete
|
Longer
|
Shorter
|
|
Best For
|
Complex medical cases, insurance-heavy documentation
|
Counseling, therapy, practices focused on efficiency
|
|
Ease for Teams
|
Requires more training, but improves clarity
|
Easier to adopt, faster for routine sessions
|
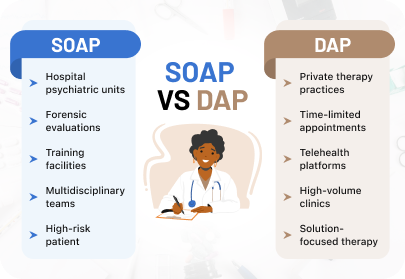
When SOAP Notes Work Best
SOAP notes are a great choice if your clinic or practice:
- Handles complex cases that need clear and detailed thinking
- Has different professionals like doctors, nurses, and therapists who work together and sharing records
- Needs to meet insurance requirements by showing a clear, step-by-step record
Example:
A physical therapy clinic helps patients recover after surgery might use SOAP notes to track each step of progress. The structured format helps both doctors and insurance companies understand what’s happening.
When DAP Notes Work Best
DAP notes are a better fit if your organization:
- Wants to save time and keep things simple
- Focuses more on therapy, counseling, or mental health, where full medical details are not always needed
- Wants staff to keep notes regularly without feeling overwhelmed
Example:
A community counseling center may use DAP notes because they are quicker to write. Therapists can include what the client said and what they noticed; all in one easy flow.
How Enquiry Medical Simplifies SOAP and DAP Notes
Choosing the right note format helps your team work smarter. Enquiry Medical’s app supports both SOAP and DAP templates, so your providers can easily switch based on the patient, specialty, or workflow.
Our app saves time by auto-filling patient information, syncing across devices, and guiding providers through each section. This ensures no details are missed and keeps your practice compliant.
Take the Next Step
Ready to cut documentation time and improve accuracy? Enquiry Medical’s flexible, user-friendly templates help your practice grow by supporting smooth workflows and better patient care.
Start today with a system designed to work the way your team does.

Dr. Conor
Conor is a Content Specialist at Enquiry Medical, where they create in-depth, accessible resources for healthcare professionals. Their writing covers a range of essential topics including clinical tools, practice efficiency, patient communication, and digital health. With a strong focus on helping practitioners stay informed and confident in their decision-making, they aim to support medical professionals at every stage of their careers. Outside of Enquiry Medical, Conor is passionate about health education, regularly contributes to wellness blogs, and enjoys exploring the intersection of technology and patient care.

 No hidden fees | Scale your practice with clear pricing and packages →
No hidden fees | Scale your practice with clear pricing and packages →